Relapse is a common part of recovery. Recognizing triggers, building coping strategies, and staying connected can help turn setbacks into growth and keep you moving forward.
Alternative formats available: Listen | Watch
Recovery from addiction is often described as a journey — a winding path with unexpected turns and moments of both challenge and growth. It’s a process that takes time, patience, and courage. Some days are easy; others are tough. One challenge along the way is relapse, which can happen to anyone on the recovery path.
In this article, we’ll break down relapse, explore the stages, offer strategies for prevention, and highlight the role of support systems. Most importantly, we’ll focus on how resilience can help you move forward, no matter what challenges arise.
Understanding Relapse: A Common Part of Recovery
Not every return to substance use is the same. Lapse and relapse are fairly common experiences in the recovery process. A lapse refers to a brief slip—such as having a drink or using a drug once—followed by an immediate return to sobriety. In contrast, a relapse involves a more sustained return to substance use after a period of abstinence. A lapse can leave individuals feeling ashamed or like a failure and the automatic response may be to hide what’s happened. After a return to substance use, individuals often have thoughts such as, “This happened because I don’t have enough will power,” or “I’m not capable of abstinence.” These thoughts may be accompanied by negative feelings, such as guilt and shame. If these thoughts are not interrupted, the likelihood that a lapse will become a relapse is increased.
A lapse isn’t a sign of personal failure; it’s often a signal that someone was overwhelmed in a difficult moment. This might happen in many different situations—like having an argument with a partner, hearing an unexpected comment, or being in a place connected to past use. It doesn’t necessarily mean someone lacks the tools to cope; sometimes, it’s just hard to use those tools in the moment. A lapse can be a chance to pause and reassess—looking at what happened, what’s helped before, and how to adjust your strategies to feel more supported moving forward.
A lapse during recovery is often seen as part of the larger change process, while a true relapse may signal a need to re-engage with more support or treatment.
Studies show that most people in recovery will experience relapse at least once. According to experts, relapse doesn’t mean you have to start over from scratch. It simply means you need to pause, reflect, and refocus on your goals. Recovery means making progress, and it’s shaped by both the challenges and the efforts to keep going.
Understanding that relapse is a part of recovery can help reduce the feelings of shame and frustration that often accompany it. Instead of feeling discouraged, remind yourself that setbacks are part of the process. The key is to get back on track and continue moving forward.
The Stages of Relapse
Relapse doesn’t usually happen suddenly. It often builds up over time, progressing through three stages: emotional, mental, and physical. By understanding these stages and recognizing early signs, you can intervene before things get worse.
Emotional Relapse
Emotional relapse starts long before any substance use occurs. During this stage, your emotions and behaviours start to shift. You might notice that you’re feeling more stressed, anxious, or overwhelmed. You may start isolating yourself from others, skipping meetings or support groups, or neglecting your self-care routines. These changes are often subtle, and you might not even realize they’re happening.
Signs of emotional relapse include:
Increased stress: Feeling overwhelmed by work, personal life, or other responsibilities.
Isolation: Spending more time alone and avoiding social situations, especially those that involve recovery activities.
Emotional imbalance: Feeling anxious, frustrated, or hopeless without reaching out for support.
Avoiding your difficult emotions or challenging situations can set the stage for future relapse. Recognizing these signs early can help you take action before things progress to the next stage.
Mental Relapse
This is when you start to experience a tug-of-war in your mind. Part of you wants to stay sober, but another part of you starts thinking about using again. You might find yourself reminiscing about the “good times” of past use or feeling tempted by old behaviours. You may start justifying risky choices or reconnecting with people or places linked to your past substance use.
Signs of mental relapse include:
Thinking about using: You might daydream about using substances, even if you’re not planning to act on it.
Rationalizing: Justifying past behaviour or convincing yourself that one slip-up won’t hurt.
Avoiding recovery activities: You may start skipping meetings or avoiding supportive people because you don’t want to confront the reality of your thoughts.
At this stage, it’s important to reach out for help, whether it’s from a sponsor, support group, or counsellor. The sooner you address these mental shifts, the easier it will be to prevent a full relapse.
Physical Relapse
Physical relapse is where you return to using substances. This is when the mental and emotional struggles result in actual behaviour — you may begin using drugs or alcohol again. While this is the most obvious stage of relapse, it’s also the most preventable if you catch the earlier signs, seek support, and adjust your coping strategies.
It’s important to remember that a physical relapse doesn’t mean your entire recovery is lost. It’s a moment to pause, reflect, and get back on track. Many people who experience physical relapse find that they learn valuable lessons about their triggers and behaviours, which helps them strengthen their recovery in the long run.
Identifying Triggers and Risk Factors
Triggers are predictable. By understanding what triggers your substance use, you can recognize your risks early, develop coping strategies, choose healthier alternatives, and stay focused on your recovery. Both external and internal triggers often overlap, so it’s important to pay attention to both. To help identify these triggers, consider the following table that outlines common external and internal triggers, as well as underlying challenges that contribute to relapse risk: Type of Trigger Description Examples Connection to Substance Use External Triggers External factors such as people, places, situations, or events that prompt memories or associations with past substance use. Walking past a bar, attending a party, hearing music tied to past use, visiting old neighbourhoods, or completing a project. Can lead to cravings and a desire to return to old habits when in familiar environments where substance use occurred. Internal Triggers Emotional or psychological states that can increase cravings when unaddressed. Stress, sadness, frustration, negative thinking, boredom, loneliness. May make individuals feel overwhelmed, prompting substance use to cope or escape emotional pain. Underlying Challenges Mental health conditions or trauma that amplify the effects of triggers. Anxiety, depression, trauma, grief, low self-esteem. These challenges can create a cycle of distress, increasing the risk of relapse without support. Common relapse triggers can also include:
Relationship Conflicts. Disagreements or tension with family members, friends, or coworkers can stir up emotions such as sadness, anger, or frustration. If not properly managed, these emotional struggles may contribute to relapse. Studies show that interpersonal conflict is involved in a large number of relapse cases.
Limited Social Support. A lack of positive, supportive relationships can make it harder to handle stress or cravings. Without a strong network, individuals may feel isolated, increasing the risk of returning to substance use.
High Stress Levels. Experiencing significant stress without healthy coping strategies can increase the temptation to return to substance use. Emotions like anger, anxiety, depression, and boredom can make it harder to resist cravings. Stress from work or relationships is often linked to relapse.
Influence from Peers. Spending time around people who use drugs or alcohol can raise the risk of relapse. Whether it's direct pressure or simply witnessing substance use, being in that environment can trigger strong urges, making recovery more difficult.
Chronic or Acute Pain. Pain from injuries, medical conditions, surgeries, or chronic illnesses/injuries can lead individuals to use prescription medications like opioids. Even when used under medical supervision, people with a history of addiction may struggle with these substances due to their high potential for dependency.
Low Confidence in Staying Sober. Believing you’re unable to maintain sobriety can increase the risk of relapse. Research shows that individuals who feel more confident about their ability to stay sober are better equipped to manage challenges during recovery.
Positive Emotional States. Surprisingly, feeling happy or celebratory can also be a trigger. Events like birthdays, anniversaries, or social gatherings might encourage substance use as a way to enhance positive emotions, leading to potential relapse.
Coping Strategies to Support Recovery
Building a toolbox of coping strategies is one of the best ways to prevent a relapse and build your resilience. Here are some effective strategies to incorporate into your recovery plan:
Mindfulness Practices. Techniques like meditation, deep breathing, and grounding exercises help you stay present and manage stress in healthier ways. One powerful approach is Urge Surfing, a mindfulness practice that teaches you to recognize and accept the feelings of an urge, rather than trying to suppress or avoid them, and to let the sensation rise and fall like a wave without acting on it. Additionally, Acceptance and Commitment Therapy (ACT) integrates mindfulness by encouraging individuals to accept difficult thoughts and emotions while committing to actions aligned with their values, helping build psychological flexibility in the face of urges and cravings.
Exercise. Physical activity not only improves your health but also boosts your mood and helps you cope with cravings.
Set Healthy Boundaries. Learning to say no, protecting your time, and distancing yourself from high-risk situations or relationships can strengthen your commitment to recovery.
Engage in Self-Care. Taking time for activities that nurture your mental, emotional, and physical health—whether it’s reading, resting, or creative hobbies—helps you build resilience.
Healthy Lifestyle Choices. Getting enough sleep, eating nutritious meals, and staying hydrated are all important for your mental and emotional well-being.
Support Networks. Staying connected with friends, family, and support groups helps you feel understood and less isolated.
Relapse Prevention Plan. Having a written plan that outlines your warning signs, coping strategies for triggers, and emergency contacts is essential to staying on track. Keep a piece of paper—or a note on your phone—with the names, phone numbers, and emails of your support network (such as a sponsor, trusted friend, or relative), along with community-based resources (e.g., inpatient or outpatient treatment programs, faith-based groups, or local community services). Having this information easily accessible helps you take steady steps forward in your recovery.
Professional support. Seeking help from a therapist or counsellor can offer specialized guidance. Therapies like Cognitive Behavioural Therapy (CBT) help individuals identify and shift harmful thinking patterns. Some may also benefit from medications that manage cravings, withdrawal symptoms, or co-occurring mental health conditions.
While these strategies are powerful tools to help you stay grounded in your recovery, it’s equally important to prepare for potential challenges. A relapse prevention plan gives you a clear roadmap for handling difficult moments and staying on track, no matter what comes your way.
Creating a Relapse Prevention Plan
Preparing for potential slips or relapse might seem counterintuitive, but it’s actually an essential part of maintaining long-term recovery. Planning ahead doesn’t mean relapse is inevitable—it means you're aware of your risks and have a clear action plan in place to address them should they arise. This proactive approach helps ensure a lapse doesn’t turn into a full relapse and gives you the tools to move forward in your recovery.
Create a detailed plan that outlines your triggers for substance use, at least three coping strategies you know help you manage stress and cravings, and a list of people in your support system you can contact for help. Consider organizing your strategies using the three stages of relapse—mental, emotional, and physical—and write specific coping tools for each. This approach helps make the plan more personalized. You may also want to include local addiction support groups. It’s important to refer to your plan regularly and adjust it over time to reflect your current needs and experiences.
The key is to have a variety of tools and strategies available to you so you can be prepared for situations that come your way. The more prepared you are, the easier it will be to stay sober.
The Role of Support Systems in Recovery
One of the most important parts of recovery is having a support system. Whether it’s family, friends, faith-based connections, or peer support groups, the people around you can make a huge difference in how you navigate recovery. Support systems offer encouragement, accountability, and a safe space to share your feelings. Staying connected through regular check-ins can remind you that you’re not alone. When you’re struggling, reaching out and asking for help can make all the difference. And maintaining open, honest communication helps build trust and understanding with those who care about you.
If you’re supporting someone in recovery, patience and empathy are essential. Listening without judgment, offering encouragement, and respecting their boundaries can go a long way in helping them stay grounded and motivated.
What to Do if Relapse Happens
If relapse does occur, it’s important to respond with compassion and understanding, both for yourself and for others. One relapse doesn’t erase all the progress made. It’s a moment to reflect, learn, and refocus on your recovery goals. Relapse often brings feelings of shame, failure, and other difficult emotions. It's okay to acknowledge them—but try to not get stuck on them, as they can get in the way of what matters most: reaching out for help. Acting quickly can make relapse a step in your recovery, not a setback.
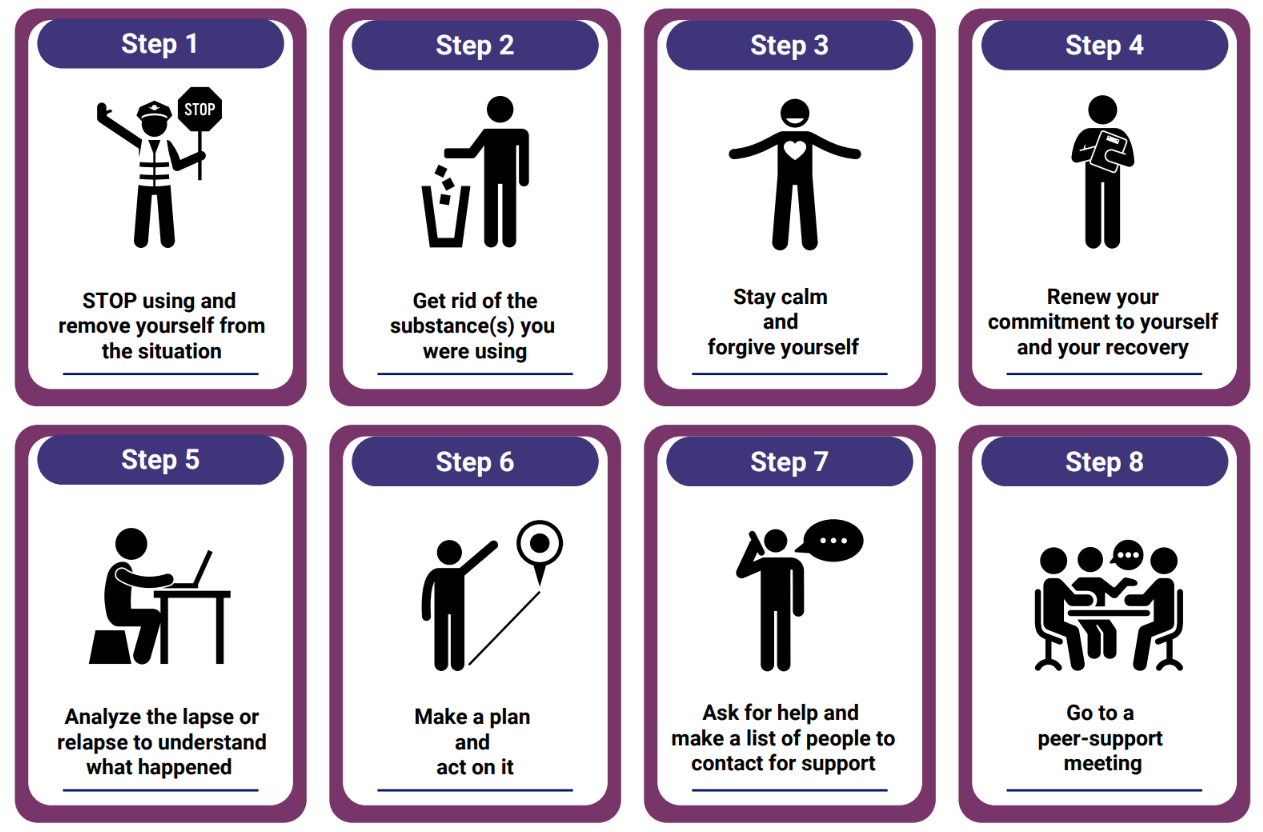
The following coping cards outline supportive actions you can take right away in the event of a relapse. They’re designed to ground you, guide you through the moment, and reconnect you with your recovery plan.
Responding quickly and with self-compassion helps you regain your footing and move forward with renewed strength — including reaching out to your support network (e.g., a sponsor, trusted friend, relative, or community-based resource).
Building a Resilient Recovery Journey
Recovery is a journey that requires resilience. Think of resilience as a muscle you’re strengthening every day. In recovery, it’s what helps you stand back up after a hard day, adapt when plans change, and keep moving forward even when the road feels rough.
Resilience in recovery means:
Celebrating progress. Each morning you stay sober, every honest chat with a sponsor, each healthy choice—these are your strength markers. Noticing them builds confidence for the next challenge.
Tolerating tough feelings. Instead of pushing away anxiety, loneliness, or frustration, you notice them (“Here’s that tight feeling in my chest”) and ride them out, knowing that feelings come and go—even cravings peak and then fade.
Learning from setbacks. Each challenge is an opportunity to grow stronger and wiser.
Practicing self-compassion and self-love. In recovery, showing yourself kindness is essential. When you catch yourself thinking negatively, like “I’ll never stay sober,” counter it with a gentler thought, such as “I’m making progress and learning every day. Every step counts.” Self-compassion helps you navigate setbacks with understanding instead of self-criticism, while self-love involves accepting and valuing yourself no matter where you are in your journey. This kinder inner voice prevents shame from taking hold, allowing you to move forward with emotional strength and a positive mindset.
Staying connected. Resilience grows when you have something to aim for: sharing a skill with your recovery group, learning a new hobby, or simply promising yourself one more day of care. Purpose fuels your determination.
Recovery is a process of self-discovery, growth, and healing. If you or someone you care about is struggling with substance use, it’s important to ask for help. Speak to your healthcare provider or local support organizations. You can also reach out to your Employee and Family Assistance Program (EFAP). You’re not alone.
References
CAMH. Fundamentals of Addiction: Preventing and Managing Relapse. Accessed 2 July 2025 from https://www.camh.ca/en/professionals/treating-conditions-and-disorders/fundamentals-of-addiction/f-of-addiction---motivation-and-change/f-of-addiction---preventing-and-managing-relapse
Guenzel, N; McChargue D. (21 July 2023). Addiction Relapse Prevention. National Library of Medicine. Accessed 2 July 2025 from https://www.ncbi.nlm.nih.gov/books/NBK551500/
Huff, C. Addiction: What to Know About Relapse. WebMD. Accessed 2 July 2025 from https://www.webmd.com/mental-health/addiction/addiction-what-to-know-about-relapse
Psychology Today Staff. (n.d.) Relapse. Psychology Today. Accessed 2 July 2025 from https://www.psychologytoday.com/ca/basics/relapse